In 1952, surgeon Roar Strøm (Figure 1) published an article detailing a case of illness in a 32-year-old man (1). Strøm had operated on the man the previous year for recurrent dyspeptic pain and discomfort. This is one of the first descriptions of the rare syndrome now known as Zollinger-Ellison syndrome (2–5) (see Box 1). We have recently confirmed the diagnosis with modern morphological techniques (6).
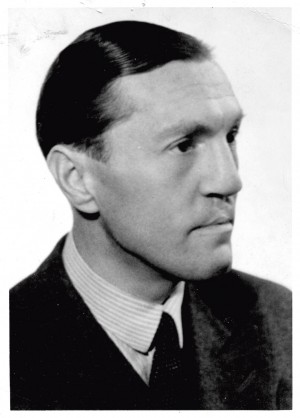
Figure 1 Dr Roar Strøm. Portrait photograph, year unknown. The copyright of the photograph is considered to have expired.
Box 1 A concise summary of Zollinger-Ellison syndrome (ZES) (4, 5)
Rare syndrome caused by one or more gastrin-producing tumours, so-called gastrinomas. The tumours are most often located in the duodenum (> 70 %), but also occur in the pancreas. Symptoms are non-specific (acid reflux, abdominal pain, diarrhoea). Recurrent or refractory peptic symptoms, or endoscopic detection of multiple ulcers or an ulcer in an unusual location (for example, the final third of the duodenum) should raise suspicion of the syndrome. Unexplained hypercalcaemia suggests possible MEN1 (multiple endocrine neoplasia type 1)-associated ZES. Measurement of fasting serum gastrin should be performed as part of the work-up of patients for whom there is clinical suspicion of the syndrome. Diagnostic imaging is mainly focused on the pancreatic area, but must also include a general oncological examination with appropriate imaging modalities. At least half of the patients have lymph node metastases, while 20–40 % have liver metastases at the time of diagnosis. Identifying patients with ZES can be challenging nowadays, partly because of the widespread use of antacids (proton pump inhibitors) among the general population, but also because serum gastrin assays vary in quality.
Today, Strøm’s name is almost forgotten, and he has not received the recognition he deserves for his pioneering description and his contributions to Norwegian medicine. He is not mentioned, for example, in the commemorative book published by the Norwegian Surgical Association to mark its 100th anniversary in 2011 (7). Our aim in this article is to present a biography of Strøm and to provide an overview of his professional achievements.
Material and method
We sought information from Stavanger University Hospital, the University of Oslo, the Norwegian Medical Association’s archives and the Regional State Archives in Stavanger, but obtained no results. We also searched the digital archives of the Norwegian newspapers Aftenposten and Stavanger Aftenblad, as well as PubMed and the Web of Science. We found the most articles in the digital archives of the National Library of Norway (bokhylla.no), using the search terms ‘senior consultant Strøm’ (in Norwegian), ‘Roar Strøm’ and ‘Hroar Strøm’. We also obtained information from Strøm’s family and from a colleague who remembers Strøm from his time in Stavanger. We investigated the handling of Strøm’s doctoral thesis using information from the archives of the Faculty of Medicine at the University of Oslo, part of the National Archives of Norway.
A difficult start
Roar Strøm grew up in the Kristiania (Oslo) suburb of Frogner, as the son of a Supreme Court lawyer. He was born with a cleft lip and palate, which apparently bothered him a good deal (Atle Aas, personal communication). He was the eldest of four children. The family was wealthy and owned several properties in the Oslo area (Atle Aas, personal communication).
In 1908, the family bought a country house in Drøbak, which they used during the summer (8). It was here that 10-year-old Roar risked his own life to save two girls of the same age, Signe and Ingeborg, from drowning in the summer of 1913. For this, he was awarded the highest honour of the Norwegian Society for Sea Rescue.
The following year, in June 1914, his father Oskar Strøm (1873–1914) was shot and killed, aged 41, in the street right by Oslo’s central station. He was shot because of his involvement – through his work as a lawyer – in a dispute between the murderer and his divorced spouse. The so-called Wiborg case attracted huge attention at the time (8) – more so than the shots that would be fired in Sarajevo only a few days later (leading to the start of the First World War). Strøm’s widow was left with four young children. The youngest was barely four months old, while Roar was the eldest at 11 years.
Roar Strøm became a student in 1920 and graduated with a medical degree from the Royal Frederick University in Oslo six years later, at only 23 years of age. It was at this time that he met Ingeborg Thygesen (1901–66), the sister of his close friend and classmate Kaare Kaarem (1899–1971). Ingeborg was divorced and had a daughter from her first marriage. Roar and Ingeborg married in 1933 and had two children together (9).
Professional activity
Strøm’s first position was as acting district physician in Ulstein in Sunnmøre. There he remained for two years prior to beginning specialist hospital training. From 1930–37, he worked as a doctor in various departments of the National Hospital in Oslo; from 1934 he was also a lecturer in surgery at the University, before being approved as a specialist in surgery in 1935 (9) (Figure 2).
Figure 2 Dr Roar Strøm in work attire, unknown time and place. The copyright of the photograph is considered to have expired.
Strøm gained broad clinical experience and training through two years as manager of the surgical outpatient clinic at the National Hospital, through private surgical practice at Vår Frue Hospital in Oslo, and from the county hospitals in Lillehammer and in Drammen, where he was senior registrar in the surgical department from 1939–42. In 1942, Strøm returned to the National Hospital as assistant physician in surgical department B. He remained there until the autumn of 1945 when, at the age of 42, he was given a permanent position as senior consultant in surgery at Rogaland Hospital in Stavanger (Figure 3).
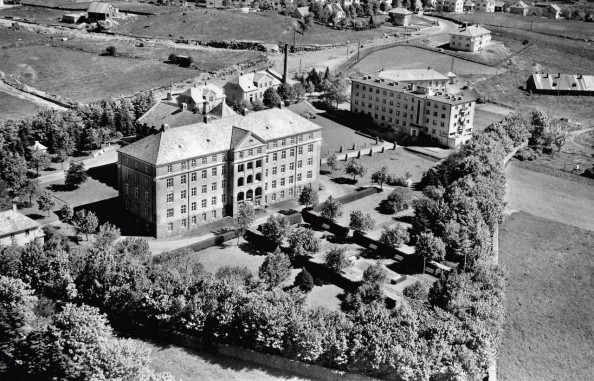
Figure 3 Rogaland Hospital photographed in 1951 by Widerøe Flyselskap [Widerøe Airlines]. The building to the right of the hospital is the Red Cross Nursing School. The white house on the right-hand side of the photograph is the old senior consultant accommodation. Photograph reproduced with the permission of Stavanger City Archives.
Strøm was highly engaged in his work as a doctor. As early as 1928, the local newspaper in Sunnmøre, where he was district physician, announced that he was going to Paris for two weeks to attend a medical congress. Almost every year throughout the 1930s we find his name on the list of applicants who received funding from ‘Malthes Legat’, a scholarship for young doctors. He reported, published, taught, researched, took part in academic meetings, and was active in the Norwegian Medical Association.
In 1933, he undertook a three-month study trip to Germany, funded by `Malthes Legat´, to learn more about modern anaesthesia. After the trip, which took in Kiel, Hamburg, Leipzig, Tübingen and Berlin, he wrote a long report on anaesthetic techniques as an update for Norwegian surgeons. He described three important methods of general anaesthesia that were new to him: nitrous oxide, tribromoethanol (Avertin), and intravenous Evipan. The article demonstrated that anaesthetic practices in Norway in the early 1930s were less advanced than those in routine use on the European continent (10).
In PubMed, Strøm is listed with only two publications (1, 11), for both of which he is the sole author. But this does not provide an accurate picture of his publishing activity. He wrote on the 25th anniversary of his time as a student that he had published approximately 25 medical articles in the academic literature on various surgical topics. His first article appeared in the Journal of the Norwegian Medical Association in 1929 and described the results of a study of school children in a fishing district in Western Norway (12). The article provides a telling socio-medical insight into living conditions in Norway in the late 1920s. Strøm reported that 22 % of the children were markedly underweight, 50–60 % had very poor teeth, and 10 % ‘had teeth that lay in ruins’.
Doctoral thesis and defence
Strøm’s research interests concerned hepatic dysfunction in patients with thyrotoxicosis. He defended his thesis on this topic in December 1942. The thesis, which was a monograph in German, was dedicated to his late father (13). It was divided into two parts and included both pathological-anatomical studies and animal experiments. The main part included studies of liver abnormalities detected in 37 autopsies, mostly performed at the National Hospital between 1913 and 1939. This work was largely undertaken over the period 1936–37. The second part was completed in the winter of 1937–38 and comprised studies of changes in liver morphology in rabbits following administration of thyroxine. This work was carried out while Strøm was an assistant in the Department of Pathology at the National Hospital.
Strøm submitted his thesis in October 1941, but more than a year would pass before he got to defend it. This was due to disagreement among the committee, which consisted of two pathologists, Georg Waaler (1895–1983) and Ole Berner (1874–1944), and one surgeon, Fredrik Roscher (1891–1962). Berner was the most critical. He wrote that the work brought nothing new, and left it to the faculty to reach a conclusion. This prompted the faculty to appoint two further members to the committee, surgeons Nils Backer-Grøndahl (1877–1975) and Ragnvald Ingebrigtsen (1882–1975), both of whom viewed the thesis in a largely positive light (14).
The official opponents in the defence were Waaler and Roscher, but it was the opposition ex auditorio that attracted attention. Surgeon Leif Efskind (1904–87), who would later become one of Norway’s leading surgeons, was hard on him. According to a newspaper report, his contribution was extremely negative in tone. Efskind thought the dissertation contained errors, and said nothing about the work’s ‘praiseworthy qualities’. To conclude his ‘long and eloquent contribution’ he presented his own unpublished results. The doctoral candidate chose not to argue back, but pointed out afterwards that he did not feel convinced by his opponent’s results (15). After the defence, the faculty obtained a copy of Efskind’s objections, which consisted of nearly 30 typewritten pages as well as several slides. Throughout the entire spring semester of 1943, the matter went back and forth between those involved. All five committee members submitted new evaluations. In late May 1943, Strøm wrote to the Dean about ‘this embarrassing and drawn-out process’. The issue had by then been discussed in three faculty meetings, and in June an end was finally put to the matter: The faculty decided by thirteen votes to three to recommend the thesis, and that same month Strøm was made Doctor of Medicine (14).
The war
Wartime would also result in a number of painful experiences. On New Year’s Eve in 1944, the British bombed the Gestapo headquarters on Victoria Terrace in Oslo, but the attack was off-target. A tram was hit and many civilians were killed. Among the 78 Norwegians who perished was Strøm’s brother-in-law, Lars Fredrik Undall (1911–44), who died at the National Hospital, where Strøm was senior registrar (16). The widow, Roar Strøm’s sister, was left with a daughter aged 15 months.
Senior consultant in Stavanger
When Roar Strøm began work as a senior consultant and head of the surgical department in Stavanger in the autumn of 1945, it was obvious that he was a competent and clinically well-trained surgeon. Like most surgeons of the time, he was a generalist whose expertise spanned the entire field. With his doctorate, he also had formal academic competence.
There were two public hospitals in Stavanger: the municipal Stavanger Hospital, which first and foremost served the city residents, and the county Rogaland Hospital, which was primarily responsible for the more rural populations of Jæren and Ryfylke area. These public hospitals were supplemented by the Norwegian Women´s Public Health Association’s maternity clinic, which was staffed by gynaecologists in private practice, and the catholic St. Franciskus hospital, run mainly by otolaryngologists in private practice. In addition, there were smaller municipal hospitals in both Sandnes and Egersund.
Strøm was a senior consultant at Rogaland Hospital, which was established in 1927. He arrived at a hospital that was still relatively modern, but which – after operating for almost 20 years – required many improvements and renovations to be “up to date”, he said, and he hoped to be able to achieve this by degrees (17). When Strøm took up his position, there were only two senior consultants in the hospital: himself in the surgical department and Roald Opsahl (1899–1980) in the medical department. Shortly after taking up his post, Strøm gave an account to the press and stated that he was already aware of the high surgical standards in Rogaland and the rich surgical traditions associated with this hospital and the district as a whole (17). He made reference to his predecessors in the city, among them senior consultant Axel Cappelen (1858–1919).
Strøm gave assurances that he was enjoying his role and said that there was a great deal to be done. Each year, about 1 500 operations were performed at the hospital, he informed them. There were five doctors in the department, and he hoped to take on another soon. The hospital had a capacity of 220–250 beds, divided roughly equally between the two departments. However, due to a shortage of doctors and nurses, it was not possible to run at full capacity (17).
The lack of nurses was a major problem. By April 1946, the nursing crisis at hospitals was apparently more severe than the public knew. There was great jubilation, therefore, when the Red Cross Nursing School opened in Stavanger that same year (18). Three years later, the first cohort graduated. Strøm was chairman of the school board, and after ten years he was able to report that the school had trained 204 nurses (19).
Strøm was also engaged in tasks outside the department. He was interested in anything that could help foster interaction between doctors working in hospitals and doctors outside. He was excited about the idea of starting a medical association in Stavanger, believing the time was ripe for such an endeavour. The association would enable colleagues to meet to discuss scientific topics and demonstrate different techniques, and would lay the foundations for close collaboration in the medical community (17).
After 10 years at the hospital, Strøm was able to look back on a great transformation. The number of patients had increased from 3 000 to 5 000 annually. The medical department had experienced growth of 60 % and the surgical department 80 %, and the number of births on the maternity ward had increased from 200 to 700 each year. The in-hospital length of stay was reduced by 50 per cent (19).
Dr Roar Strøm also became involved in the local community. He gave lectures for the general public on topics including blood transfusions, degenerative disorders of the legs and back, and cancer treatment. There was discussion at that time too about the organisation of the healthcare system and the location of hospitals. In a lecture at Bethania prayer house in 1948, then the largest venue in Stavanger, he spoke in favour of centralising hospitals in Rogaland, in order to create institutions and communities that could benefit from medical innovations requiring technical, financial and administrative resources. According to a newspaper report, the prayer house was almost full and the senior consultant was rewarded with loud applause after his lecture (20).
Strøm could also adopt more unconventional methods, such as the time in 1946 when he invited two journalists for a drive so that he could show them the road to the hospital. It was in appalling condition. Being transported along this “washboard road” was agony for patients, and had been so for many years (21). He made his opinions known, too, about other matters he considered deserving of criticism. In 1949 he wrote an indignant letter to the local newspaper about a group of young people who had behaved “disgracefully” during a service in the cathedral (22). He was certainly widely engaged.
Dr Strøm was also easily recognisable in Stavanger when out driving his car – a large, yellow American model (Reidar Vik, personal communication). As a hobby, he wrote that he dabbled in “a little portrait sketching and watercolour painting” (23).
Pioneering work
In December 1952, Strøm published an article detailing the medical history, diagnosis, treatment and morphological findings for a 32-year-old man from Jæren. The patient had had stomach problems for several years. In 1948, he had undergone a partial gastrectomy, in 1950 a bilateral thoracic vagotomy and in April 1951, Strøm performed a subtotal gastrectomy and distal pancreatectomy (1). After the operation, the patient felt like new. His unrelenting stomach pain had completely disappeared. Strøm’s article was published in Acta Chirurgica Scandinavica in December 1952 (1).
Strøm’s case history has recently been checked and evaluated by Søreide and Lea (6). The information in the 1952 article was entirely consistent with the information in the medical records. Strøm’s last information on the patient was obtained at a 13-month follow-up in May 1952. However, the patient subsequently deteriorated, with recurrent epigastric pain, vomiting and weight loss, and he died in April 1953 at Rogaland Hospital, 24 months after the operation (6).
With the aid of modern morphological techniques, including immunohistochemistry, Søreide and Lea were able to confirm that the patient had a functional neuroendocrine tumour in the pancreas, consistent with a gastrinoma (6), as we understand the condition today (4). Strøm himself had detected liver metastases in the patient, and an examination of formalin-fixed tissue from 1953 confirmed the presence of liver metastases from a gastrinoma (6).
In April 1955, just over two years after Strøm had published his article, American surgeons Robert M. Zollinger (1903–92) and Edwin H. Ellison (1918–70) presented two patients with hypersecretion, hyperacidity and atypical peptic ulcer associated with a non-insulin-producing pancreatic islet cell tumour. They considered their findings, which they presented at the congress of the American Surgical Association in Philadelphia, to reflect a new disease entity and assumed there was a connection between the findings, although they did not know what it was. In October that same year, their observations were published in the Annals of Surgery (2), and only the following year Eiseman and Maynard proposed naming the condition ‘Zollinger-Ellison syndrome’ (3). A search for ‘Zollinger-Ellison syndrome’ in PubMed now results (as of 22.2.2019) in over 3 500 hits, dating back to 1956, and the disease is often referred to by the three-letter acronym ‘ZES’.
When Zollinger and Ellison presented their findings, it became clear that similar observations had been made previously. A few single case reports from the USA and Europe were published in the first half of the 20th century (24, 25), but these were not interpreted as reflecting a single condition, and there is some uncertainty over the diagnosis owing to the limited clinical information (24).
Strøm provided a comprehensive and detailed description of his patient, but his article was not cited by Zollinger and Ellison. However, his contribution was quickly recognised by his Nordic colleagues (26, 27), and the term Strøm-Zollinger-Ellison syndrome is used occasionally. Although this search term results in only four hits in PubMed, it is used in the online Norwegian medical dictionary ‘Store medisinske leksikon’ as well as the eponym database ‘Whonamedit?’, and yields additional hits in a general internet search.
According to the Web of Science citation database, Eiseman and Maynard were the first to cite Strøm’s article (3). The following year, in 1957, the syndrome was mentioned – and Strøm’s article cited – in an editorial in The Lancet (28).
Following the publication of his article in 1952, a number of Strøm’s foreign colleagues contacted him to discuss the details or to obtain further information. Some of these enquiries came after Strøm had left Stavanger, and others after his death. This correspondence can be found in the patient’s hospital record.
Zollinger and Ellison were not the first to describe the syndrome, but their names have nevertheless been linked to it. This is true of many eponyms. It is not always those who are first to describe a condition who get the credit. In this case, it was Eiseman and Maynard who came up with the idea for the name, probably to honour their colleagues, but perhaps also to simplify the description of the syndrome (3).
A difficult end
Strøm continued to be active in his profession. In April 1955, the newspaper Nordisk Tidende reported that he was to spend two months in the USA, mostly at the Mayo Clinic in Rochester, Minnesota (29). While in the USA, he visited many pulmonary clinics, later writing that he was very surprised not to have seen a single thoracoplasty performed by the clinics he visited. The Americans carried out only intrathoracic procedures (11). Strøm had a great interest in thoracic surgery and, in August 1957, he published the results of ten years of pulmonary tuberculosis surgery in Stavanger from 1946–56, a total of 713 operations on 508 patients (11).
In August 1955, the senior consultant position at Telemark county hospital in Skien was advertised as vacant. The advertisement stated that the hospital was a ‘mixed hospital’ with 120 beds, mostly for surgical patients (30). Only two months later, the local newspaper was able to announce that Strøm had been given the position. The newspaper assured readers that Strøm ‘enjoys a great reputation as a skilled and conscientious doctor’ (31). Perhaps Strøm had envisaged a somewhat slower pace at the smaller hospital in Skien. He took up the position in July 1956, but the initial period was arduous. After three months, he stated that there was a critical shortage of doctors at the hospital (32). Two doctors – himself and a registrar – had to take care of about 100 inpatients, something he described as an almost hopeless task. It was impossible for two doctors to manage the workload, especially with the need for night shifts. The shortage of doctors was a result of the hospital being unable to attract suitable candidates because it had no separate medical department. Doctors were not interested in working in such places. It is a disgrace that the county hospital in Skien does not have such a department, Strøm said, and argued that a medical department must be established as soon as possible (32).
Shortly afterwards, however, his health began to decline, and only the following year he had to withdraw from employment (33). Roar Strøm died in October 1958, aged just 55 years.
Legacy
Strøm’s comprehensive article was based on a single patient. His observations and descriptions were impressive, even though knowledge of the condition’s pathophysiology was, unsurprisingly, limited. Strøm was aware that there had been reports in the scientific literature from the late 1920s of hypoglycaemia caused by excess insulin secreted by a pancreatic tumour. Such tumours were referred to at the time as insulomas; today the term insulinomas is generally preferred. However, Strøm’s patient had not had symptoms of hypoglycaemia, and Strøm therefore considered the tumour to be a non-functional insuloma. He believed the concurrence of the insuloma and stomach ulcer to be an incidental one-off event (1), whereas Zollinger and Ellison were bolder and suggested in their article that an ulcer-causing factor in the pancreas could explain the condition. They assumed that glucagon might be the active agent (2). It was not until 1967–15 years after Strøm’s article – that Gregory et al. detected gastrin in a tumour extract from a patient with Zollinger-Ellison syndrome, thereby establishing the pathophysiological association between a gastrin-producing pancreatic tumour – a gastrinoma – and the clinical symptoms and findings associated with this syndrome (34).
Strøm had no doubt that the patient on whom he had operated was a special case. As far as we know, the article from 1952 was his only publication in English. He wrote that his reason for publishing the case history was not so much because of this unusual condition, but rather because this case of illness could point to, and perhaps shed light on, issues of great medical importance, both theoretical and practical (1).
Although Zollinger and Ellison made their own observations from their two patients, their insights were hardly double those of Strøm, who had only a single patient. But what all three surgeons had in common was that they dared to present something they did not fully understand.
Roar Strøm was a clinically experienced and hard-working surgeon with academic expertise. He worked as a surgeon for over 25 years, and has left a clear legacy in Norwegian medicine. No-one has written his biography before, and we feel it is only right that his contribution should be highlighted. Honour has no expiry date – at least not when it is deserved.
