Rotavirus is the most frequent cause of severe diarrhoea in small children (1). In the period 2006–13, rotavirus was the cause of 63–65 % of all gastroenteritis-related hospital admissions in children under five years of age. Most cases were found at age 6–23 months, and the frequency was highest in the first and second quarters of the year (2, 3).
We have no similar surveys of rotavirus infections in general practice, but several assessments of gastroenteritis, vomiting and diarrhoea, based on electronic reimbursement claims from GPs and doctors in the emergency primary health care units, have been conducted (3–5). Gastroenteritis is the cause of 3.6 % of all consultations in relation to children under five years of age (5). The distribution of consultations is 28–30 % at the emergency primary health care units, with the remainder taking place at GP offices (3–5). Prior to the introduction of the rotavirus vaccine, it was estimated that almost 30 % of the cases were due to the rotavirus (1, 2).
In 2014, the rotavirus vaccine was included in Norway’s Childhood Immunisation Programme and is offered to all children born after 1 September 2014. The aim of this study was to map emergency primary health care consultations due to gastroenteritis before and after the introduction of the rotavirus vaccine.
Material and method
The material consists of data from all electronic reimbursement claims that were submitted by emergency primary health care doctors in the period 2010–18, which had previously been used to compile the annual statistics for the emergency primary health care services (Årsstatistikk fra legevakt) (6). Anonymised computer files were obtained from the Norwegian Health Economics Administration/Control and Payment of Reimbursement to Health Service Providers (KUHR).
Consultations and home visits (tariff codes 2ad, 2ak, 2fk, 11ad or 11ak, herein referred to as consultations) were recorded for children aged 0–4 years. The consultations coded with diagnostic codes D70 (gastrointestinal infection) or D73 (gastroenteritis, presumed infection), were included.
It is impossible to specifically identify rotavirus infections in such a dataset, but most children with rotavirus are probably included in these two diagnostic codes. Changes in consultation rates in relation to these diagnoses will therefore reflect changes in the number of consultations due to rotavirus infections.
As a main rule, doctors must use diagnostic codes, but in some cases uncertainty may lead to the use of less specific symptom codes, e.g. D10 (vomiting) or D11 (diarrhoea). If such codes are included, the dataset will comprise several other conditions, particularly among the youngest children. Changes in consultation rates will then reflect changes due to rotavirus infections to a smaller degree. For example, the annual consultation rate for 2015–16 declined from 22 to 19 per 1000 inhabitants for diagnostic codes D10/D11 and from 22 to 12 for D70/D73 (age group 0–2 years).
Consultation rates were calculated for each quarter, and for each age group in the 0–4-years range, using the number of inhabitants according to Statistics Norway as the common denominator. The consultation rate ratio for the years 2015–18 was calculated by dividing the consultation rate by the corresponding mean for the years 2010–13 (prior to the introduction of the vaccination programme).
Vaccination coverage was obtained from the Norwegian Immunisation Registry (SYSVAK) (7). This states the annual number of two-year-olds who have been fully vaccinated against rotavirus. Such figures are available from 2017 and therefore largely include all children vaccinated in 2015. Vaccination coverage among two-year-olds is given as 91.9 % in 2017 and 92.8 % in 2018.
The annual statistics for the emergency primary health care service were assessed by the Norwegian Labour and Welfare Administration’s data protection officer and by the Data Protection Official for Research (6). Because it is impossible to identify individuals on the basis of the material, be it directly or indirectly, the project is not subject to the notification requirements imposed by the Norwegian Personal Data Act.
Because the material comprises all the electronic reimbursement claims rather than a sample, the differences demonstrated are real and not encumbered by statistical uncertainty. The data are therefore presented without confidence intervals, and no statistical tests have been conducted.
Results
Figure 1 shows quarterly consultation rates for the period 2010–18, distributed across each individual age level. The regular peaks occur in the first quarter of each year. A clear reduction is seen in the rates for the first quarter of 2016, one year after vaccination began.
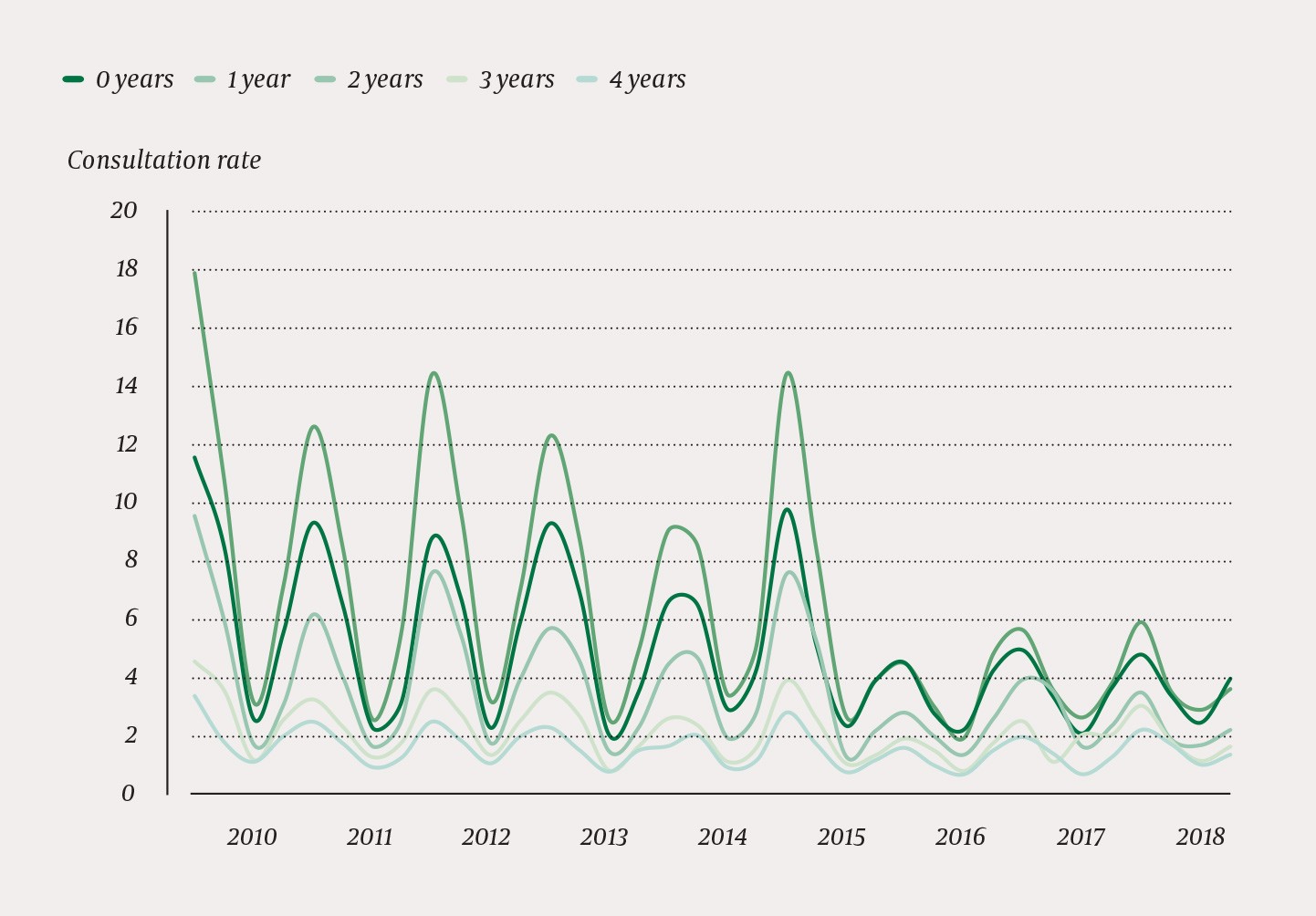
Figure 1 Quarterly consultation rates (per 1000 inhabitants) at the emergency primary health care units for children aged 0–4 years in the years 2010–18. The diagnoses are D70 (gastrointestinal infection) or D73 (gastroenteritis, presumed infection). Vaccination against rotavirus commenced in the fourth quarter of 2014.
Table 1 shows the consultation rate ratio for each quarter in the years 2015–18, compared with the corresponding mean for the years 2010–13. Vaccinated age groups are highlighted in bold in the table. The decrease in consultation rates is greatest in the first and second quarters, and least in the third quarter. The decrease is not limited to vaccinated age groups.
Table 1a
Gastroenteritis-related consultation rates in a period prior to vaccination against rotavirus (2010–13). Mean consultation rate per 1000 inhabitants for the years 2010–13.
|
Year and quarter
|
|
|
|
Age
|
|
|
|
|
0 years
|
1 year
|
2 years
|
3 years
|
4 years
|
|
|
1.
|
|
9.7
|
14.3
|
7.3
|
3.7
|
2.6
|
|
|
2.
|
|
7.2
|
9.5
|
5.0
|
2.8
|
1.7
|
|
|
3.
|
|
2.3
|
2.9
|
1.6
|
1.1
|
0.9
|
|
|
4.
|
|
4.5
|
6.2
|
2.9
|
2.1
|
1.6
|
Table 1b
Consultation rate ratio for the years 2015–18 (after vaccination against rotavirus), calculated by dividing the consultation rate by the corresponding mean for the years 2010–13. The numbers in bold indicate the years and age groups included in the vaccination programme.
|
Year and quarter
|
|
|
|
Age
|
|
|
|
|
0 years
|
1 year
|
2 years
|
3 years
|
4 years
|
|
2015
|
|
|
|
|
|
|
|
|
1.
|
|
1.0
|
1.0
|
1.0
|
1.0
|
1.1
|
|
|
2.
|
|
0.7
|
0.9
|
1.1
|
0.9
|
1.0
|
|
|
3.
|
|
1.0
|
0.9
|
0.8
|
0.9
|
0.8
|
|
|
4.
|
|
0.9
|
0.6
|
0.7
|
0.6
|
0.7
|
|
2016
|
|
|
|
|
|
|
|
|
1.
|
|
0.5
|
0.3
|
0.4
|
0.5
|
0.6
|
|
|
2.
|
|
0.4
|
0.3
|
0.4
|
0.5
|
0.6
|
|
|
3.
|
|
1.0
|
0.7
|
0.8
|
0.7
|
0.7
|
|
|
4.
|
|
0.9
|
0.8
|
0.9
|
0.8
|
0.9
|
|
2017
|
|
|
|
|
|
|
|
|
1.
|
|
0.5
|
0.4
|
0.5
|
0.7
|
0.7
|
|
|
2.
|
|
0.5
|
0.4
|
0.7
|
0.4
|
0.8
|
|
|
3.
|
|
0.9
|
0.9
|
1.0
|
1.8
|
0.7
|
|
|
4.
|
|
0.8
|
0.6
|
0.8
|
1.0
|
0.8
|
|
2018
|
|
|
|
|
|
|
|
|
1.
|
|
0.5
|
0.4
|
0.5
|
0.8
|
0.8
|
|
|
2.
|
|
0.5
|
0.4
|
0.4
|
0.6
|
1.0
|
|
|
3.
|
|
1.1
|
1.0
|
1.0
|
1.0
|
1.0
|
|
|
4.
|
|
0.9
|
0.6
|
0.7
|
0.8
|
0.8
|
Discussion
In line with other studies, our dataset also shows typical seasonal fluctuations with the highest incidence in the first quarter of the year (2, 3, 5). The consultation rate is highest in the 0–2 years age group, with one-year-olds at the very top. This distribution is very similar to that previously shown for rotavirus infections in hospitals (2, 3).
Vaccination began in October 2014, so relatively few children had been vaccinated at the start of the 2015 sickness season. The gastroenteritis-related consultation rate was at least as high in 2015 as the previous years.
However, from 2016 onward, a clear reduction in the consultation rate can be observed. In particular, the sickness peaks in the first and second quarter have declined, first and foremost for the 0–2 years age group. This is to be expected based on previous knowledge of the spread of rotavirus (2, 3).
Notably, there is a significantly reduced incidence in unvaccinated two-year-olds in 2016, which may indicate that the vaccine gives a certain degree of herd immunity. Older children appear to benefit less from the vaccine. It is likely that the incidence of rotavirus is lower in these age groups.
Statistics Norway states that since 2012, the consultation rate for children aged 0–5 years at the emergency primary health care units has been gradually falling, while the corresponding consultation rate at GP offices has remained stable (8). However, the reduction in gastroenteritis-related consultation rates is of a very different order of magnitude and has taken place over a shorter period of time.
Conclusion
Since 2016, emergency primary health care consultations due to gastroenteritis in small children have sharply declined. This is related to the introduction of the rotavirus vaccine in the Childhood Immunisation Programme on 1 October 2014. Nevertheless, we cannot conclude that there is a confirmed causal relationship.
